Morrisville, NC – March 4, 2022 – Before Alexander Fleming discovered penicillin, another more selective antibacterial agent rose to popularity in the early 1900s: bacteriophage.
In 1917, microbiologist Felix d’Herelle was tasked with identifying the cause of a dysentery outbreak impacting French troops. From his research, he noticed that Shigella bacteria was the primary culprit of this affliction. He then discovered an invisible microorganism that targeted and eliminated the dysentery bacillus, or rod-shaped bacteria, which he eventually named ‘bacteriophage’ (also known by the shorthand ‘phage’) for its supposed bacteria-eating capabilities. D’Herelle would later apply this knowledge to successfully treat children suffering from severe dysentery at the Hospital des Enfants Malades in Paris and create cures for other pathogens like cholera and typhoid. Encouraged by d’Herelle’s contributions and similar studies, there was soon overwhelming excitement surrounding phage therapy and its success in curing infectious diseases. In fact, this precision approach garnered so much attention that d’Herelle and George Eliava co-founded an institute in Tbilisi, Georgia, in 1923 that was dedicated to studying bacteriophages and clinical use of phage therapies. However, this movement’s momentum quickly fizzled out after the discovery of the first antibiotic, penicillin, in 1928.
Phage therapy fell out of favor with scientists, physicians and the public in the 1930s and 1940s primarily due to the uncertain biology behind bacterial viruses – which wouldn’t be studied in detail until the invention of the electron microscope – and the widespread availability and convenience of antibiotics in the early post-World War era. These miracle drugs could be prescribed broadly by physicians to cure a plethora of ailments without identifying the specific pathogenic strain. In stark contrast, phage therapies required isolation of specific phages to treat each bacterial pathogen, specific diagnosis of the pathogen afflicting each patient, and a much more complex manufacturing process than that required to produce antibiotics on an industrial scale. Together, these factors undermined the potential of targeted medicine and phage therapy research. Hence, the beginning of the golden age of antibiotic discovery.
The need for precision medicine
The emergence of antibiotics created modern medicine, yielding a massive epidemiologic transition: developed countries transitioned from populations with high mortality rates attributed to communicable diseases to skyrocketing life expectancies. Ironically, this shift in life expectancy increased the prevalence of chronic illnesses. Yet, this ‘one-size-fits-all’ approach to treating bacterial pathogens set us on an inevitable path to the evolution of even deadlier pathogens. While broad-spectrum antibiotics are excellent at obliterating harmful bacteria, they also indiscriminately eliminate beneficial bacteria in the body. Furthermore, the use of these medicines creates selective pressures on bacteria that favors the emergence of bacterial strains that are resistant to antibiotics, a phenomenon known as antimicrobial resistance (AMR). Naturally, the biopharmaceutical industry continued to develop natural and synthetic antibiotics that were stronger and better than their predecessors. However, as these medicines progressively became more potent at killing bacteria – both bad and good – they often also became increasingly toxic. Unfortunately, bacteria have intrinsic resistance mechanisms that are effective against weaker antibiotics and can rapidly evolve to evade the strongest antibiotics – creating more problematic bugs down the line.

Figure: The Kishony MEGA plate experiment from 2016 provides a cinematic demonstration of bacterial capabilities to evolve resistance across varying concentrations of antibiotics. From the edges moving inward, each colored band represents a tenfold increase in antibiotic concentration. Within only 11 days, the E. coli bacteria managed to reach the center, gaining 1000x greater antibiotic resistance than they had at the start of the experiment.
More information on the MEGA plate experiment is available on Research Gate.
Today, we have ten different classes of antibiotics, organized by their chemical and pharmacological characteristics, with well over 100 FDA-approved drugs. Yet even our best and strongest anti-infectives can be thwarted by AMR strains. With high costs, low returns and few financial incentives, multiple large pharmaceutical companies exited the antibiotic sector. Several smaller companies went bankrupt after commercializing new antibiotics that were undifferentiated from their predecessors and were therefore rarely used. As a result, the pipeline of new antibiotics has dried up at the same time that antibiotic resistance rates are rising dramatically (a recent analysis of AMR global burden published in The Lancet found almost 5 million estimated deaths associated with bacterial AMR in 2019), creating an urgent need for novel solutions.
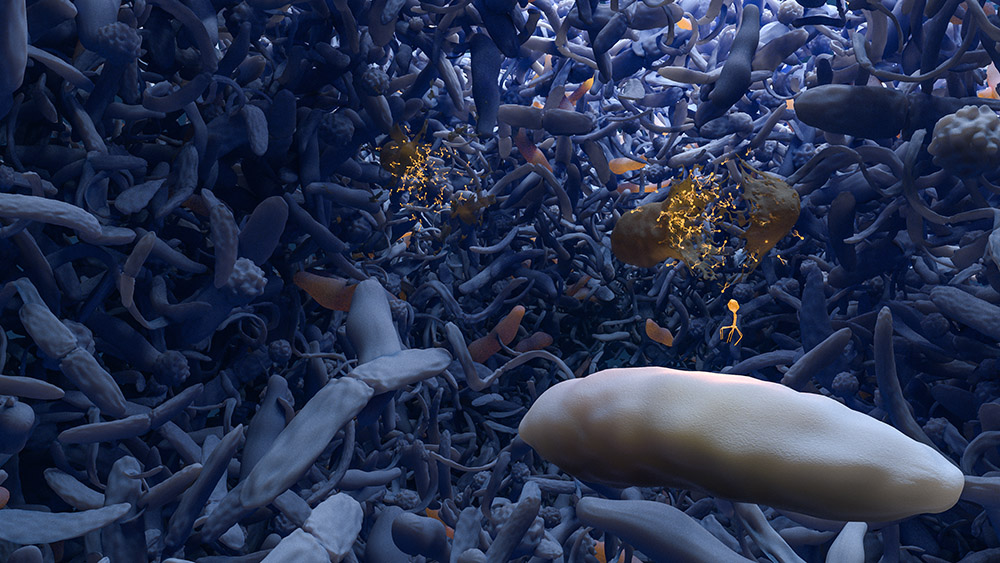
Enter precision medicine. Similar to the way that targeted treatments have revolutionized cancer therapy, displacing non-specific and highly toxic treatments like chemotherapy and radiation, precision antibacterial therapy provides patients with treatment for the particular bacterial pathogen causing their infection. More specifically, phage therapy has regained favor with scientists, clinicians and entrepreneurs because of two driving factors: 1) its unprecedented ability to target bad bacteria while sparing good bacteria, avoiding the selective pressure to non-target bacteria that often results in AMR; and 2) decreased cost in sophisticated genomic sequencing and related technologies that support high-throughput bacteriophage isolation and characterization. There is now a strong and growing belief that these precision biotherapeutics should be leveraged in conjunction with antibiotics to combat infections, particularly those that have become resistant to traditional antibiotics.
Locus’ approach to precision medicine and phage therapy
Locus believes bacteriophage therapy represents a sustainable solution to the AMR crisis and will soon begin to augment antibiotics in the treatment of bacterial infections. By engineering our products with CRISPR-Cas3, we have overcome the weaknesses of natural phage therapy. As a result, we are developing medicines for four of the most prevalent AMR pathogens with efficacy equivalent to or better than standard of care antibiotics. In 2021, Locus completed the world’s first clinical trial with CRISPR-Cas3 enhanced bacteriophages for lead candidate LBP-EC01 targeting E. coli bacteria causing urinary tract infections. The trial met its primary and secondary endpoints and demonstrated safety and tolerability.
Much like how targeted therapies revolutionized cancer treatment, we expect our “one bug, one drug” approach will eventually displace antibiotics as first-line therapy while preserving the antibiotic armamentarium for use as a last resort.
In addition, based on decades of research, we understand bacteria play crucial roles in many aspects of human health, including infection and inflammation. We are developing our technology for applications beyond infectious disease to target pathogenic bacteria that have a role in causing or exacerbating diseases across multiple therapeutic areas. We believe phage therapy has an exciting future in battling the global ‘silent pandemic’ in AMR and beyond.
